Ultrasound and MRI have long been the go-to methods for monitoring and diagnosing liver steatosis, but a recent meta-analysis suggests that non-contrast computed tomography (NCCT) could serve as a promising alternative for detecting moderate levels of this condition. Published in the journal Radiology, the study assesses the effectiveness of NCCT along with contrast-enhanced CT (CECT) and dual-energy CT (DECT) in diagnosing hepatic steatosis through an analysis of 42 studies that involved 14,186 participants.
The findings were quite revealing: NCCT demonstrated a sensitivity of 72% and specificity of 88% in identifying steatosis where more than 5% fat was detected in biopsy results. These figures were quite comparable to CECT, which had a sensitivity of 66% and specificity of 90%. Interestingly, DECT stood out with an improved sensitivity of 85% and matching specificity of 88%.
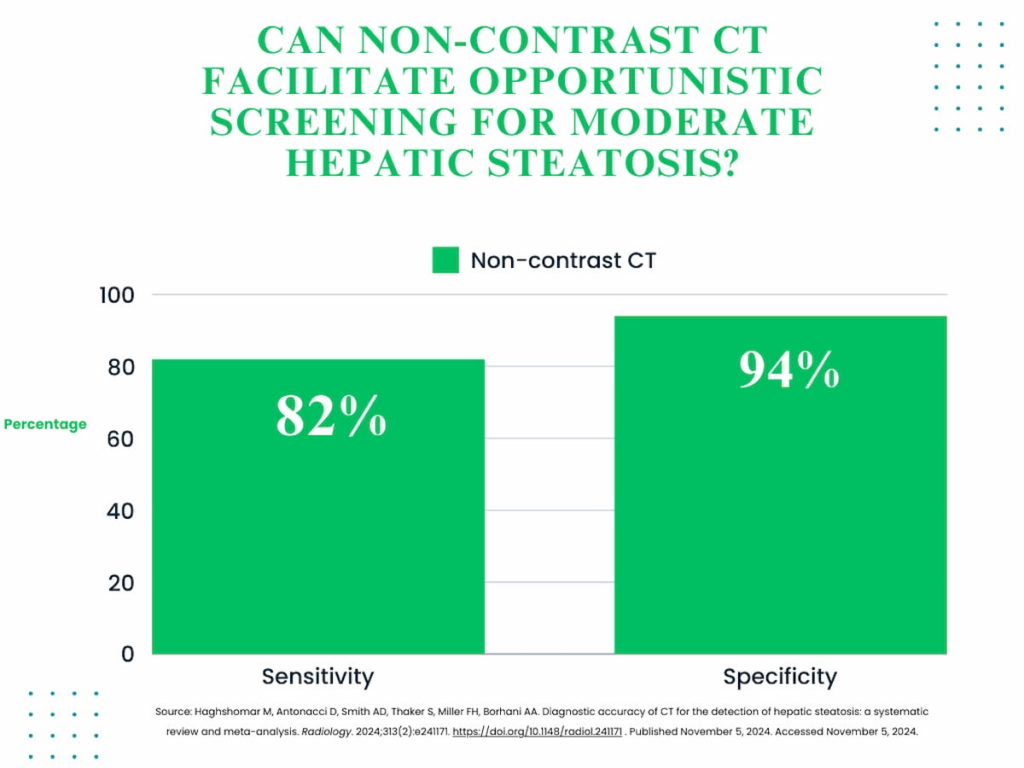
For individuals displaying moderate hepatic steatosis—defined as having 20 to 33 percent fat as revealed in biopsy—NCCT exhibited a sensitivity of 82% and specificity of 94%. This is in stark contrast to CECT, which showed a lower sensitivity of 68% while maintaining similar specificity at 93%.
Dr. Maryam Haghshomar of Northwestern University Feinberg School of Medicine led the meta-analysis and noted that while NCCT is not typically used for screening, it plays an essential role in the incidental detection of steatosis during scans conducted for other medical reasons. Such opportunistic findings could prompt further clinical evaluations and tests to discern risk factors for more severe liver conditions, necessitating advanced treatment.
The study authors also brought attention to specific diagnostic indicators associated with better accuracy. For instance, high specificity in diagnosing moderate hepatic steatosis was evident when absolute liver attenuation was under 40-45 Hounsfield Units (HU), when the liver-spleen attenuation ratio measured less than 0.9-1, or when the difference between liver and spleen attenuation was less than -5 to 0 HU.
While NCCT shows potential in opportunistic screening for steatosis, several factors remain in play. Dr. Haghshomar and her research team noted that differences between liver and spleen attenuation appeared to be the most consistent indicator for NCCT. This parameter was thought to be less influenced by variations in CT equipment settings, such as tube voltage and scanner type.
Despite promising findings for NCCT, challenges persist in fully validating these modalities. A subgroup analysis revealed extremely high specificity for CECT and DECT—at 99% and 93%, respectively. However, the researchers acknowledge that due to the small number of studies focusing on these methods, and the resulting inconsistency in reference standards, drawing a definitive conclusion remains difficult.
Limitations of the meta-analysis include the absence of a consistent threshold for defining moderate steatosis. Additionally, changes in CT techniques and technologies over the 26-year span during which the reviewed studies were conducted introduce another layer of variability in the results.
This exploration into the potential of NCCT could have significant implications for its use in clinical settings, particularly in contexts where MRI or ultrasound might not be readily available. Thus, while NCCT may not replace these standard screening tools outright, it holds promise for enhancing the detection and management of hepatic steatosis, especially when integrated into existing diagnostic pathways.