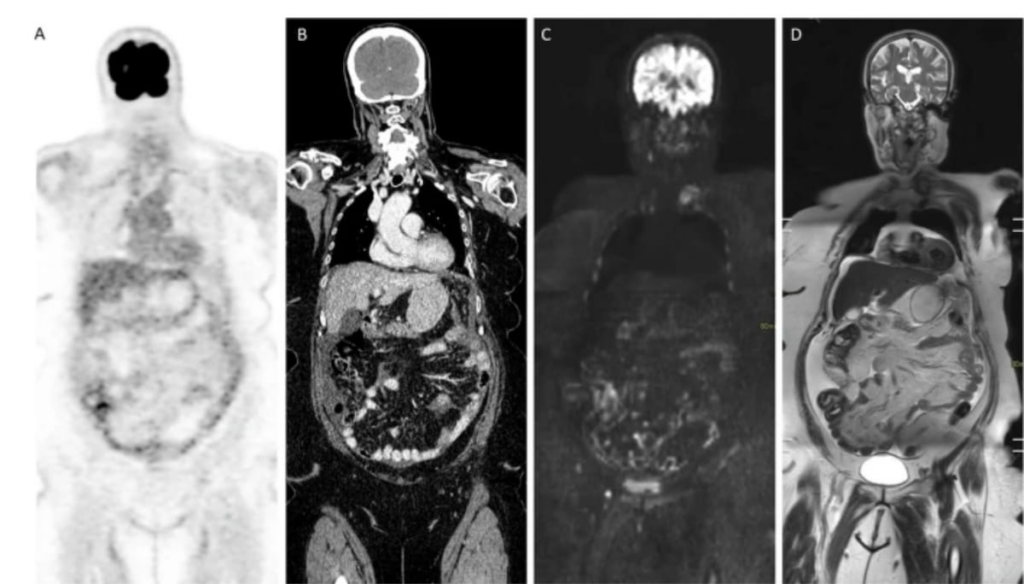
In addressing the best imaging techniques for diagnosing peritoneal metastases, particularly in patients with colorectal or ovarian cancer, recent research has offered new insights. Published in European Radiology, these guidelines are the result of collaboration among the European Society of Gastrointestinal and Abdominal Radiology, the European Society of Urogenital Radiology, the European Association of Nuclear Medicine, and the Peritoneal Surface Oncology Group International. These guidelines elucidate the strengths and limitations of various imaging modalities, notably discussing the role of CT, PET/CT, and DWI-MRI.
Initially, the standard CT scans, often employed during the first evaluation of ovarian and colorectal cancer, are scrutinized for their limitations in detecting peritoneal metastases. Particularly in the context of small bowel and abdominopelvic lesions, CT scans show questionable accuracy. This is especially evident when dealing with lesions smaller than one centimeter located in difficult-to-assess areas such as under the diaphragm and around the omentum, serosa, and mesentery, particularly when ascites is present. This analysis led researchers to underline the inadequacy of CT in effectively staging peritoneal metastases under these conditions.
In contrast, diffusion-weighted imaging magnetic resonance imaging (DWI-MRI) using Short T1 Inversion Recovery (STIR) showcases significantly improved accuracy compared to CT and FDG PET/CT, especially for small lesions. This makes DWI-MRI a superior method for site-specific analysis of peritoneal metastases. It is particularly useful for assessing patients with sub-centimeter lesions, providing a deeper understanding and clearer imaging of metastases spread.
In terms of planning treatment for colorectal cancer patients, particularly those preparing for hyperthermic intraperitoneal chemotherapy (HIPEC), abdominal DWI-MRI appears more beneficial than CT. This advantage becomes apparent in diagnosing abdominopelvic extraperitoneal metastases, offering a clearer, more accurate picture that can guide therapeutic decisions.
One significant challenge posed by CT in managing peritoneal metastases is its difficulty in assessing varying manifestations and calculating the peritoneal cancer index (PCI). According to a meta-analysis cited by the guideline authors, CT can lead to an underestimation of surgical PCI by as much as 12 to 33 percent. In contrast, DWI-MRI displays a strong correlation with surgical PCI, suggesting its superiority in accurately detecting peritoneal metastases, particularly in recurrent cases in ovarian cancer as well as initial and subsequent colorectal and ovarian cancer assessments.
Exploring the use of FDG-PET/CT, researchers noted its high sensitivity (87 percent) and specificity (92 percent) for detecting peritoneal metastases. However, the method is significantly limited by its inefficiency in identifying small lesions and hypometabolic metastases, which impairs its reliability in preoperative staging.
The ability of DWI to suppress background signal from organs and ascites is highlighted in the guidelines, noting that using a STIR pre-pulse rather than a spectral attenuated inversion recovery (SPAIR) pre-pulse enhances the effectiveness of DWI sequencing. This improvement is crucial for large-volume body imaging and significantly aids in the detection of serosal metastases.
Finally, STIR-DWI-MRI stands out for its capabilities in assessing post-neoadjuvant chemotherapy progress, evaluating tumor recurrence, and determining the suitability of patients for cytoreductive surgery. This imaging modality is deemed to offer unparalleled accuracy in understanding the extent of peritoneal metastases in patients suffering from ovarian or colorectal cancers.