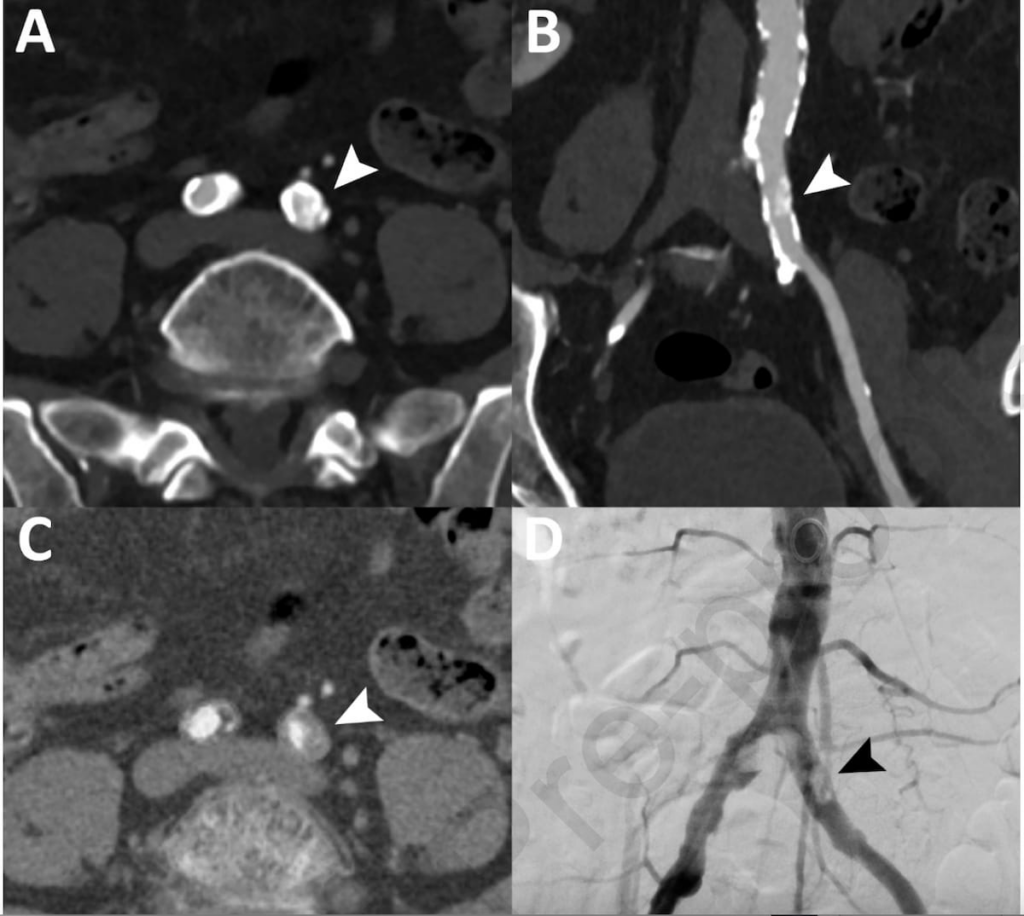
Recently, researchers have been exploring the effectiveness of a new imaging technology called photon-counting computed tomography angiography (PC CTA) as a potential non-invasive method to identify stenotic lesions in patients suffering from peripheral artery disease (PAD). Traditionally, diagnoses of such conditions have relied on digital subtraction angiography (DSA), an invasive procedure that provides detailed images of blood vessels. The study, published in the European Journal of Radiology, examines whether PC CTA could serve as a reliable alternative to DSA.
In this retrospective analysis, the researchers scrutinized data from 109 patients, with a median age of about 75, who had undergone both PC CTA and DSA. The study also evaluated photon-counting (PC) pure lumen reconstruction data from 91 of these patients. Altogether, the team assessed 933 vascular segments using PC CTA, and they reviewed 780 segments through PC pure lumen reconstructions.
Findings from the study revealed that PC CTA demonstrated impressive diagnostic capabilities, showcasing a 91 percent sensitivity, 95 percent specificity, and 93 percent accuracy in pinpointing stenotic disease. The PC pure lumen reconstructions showed slightly lower rates, with 85 percent sensitivity, 89 percent specificity, and 88 percent accuracy.
Lead author Dr. Patrick Ghibes, from the Department for Diagnostic and Interventional Radiology at University Hospital Tubingen, highlighted that the study’s results indicate PC CTA as an excellent technology for detecting high-grade vascular stenosis. Its high accuracy makes it a valuable non-invasive option for diagnostic and treatment planning in patients dealing with symptomatic PAD.
The challenge of distinguishing between vessel calcifications and true intravascular contrast in smaller-diameter vessels, such as those found in the calf area, has long troubled medical professionals. However, the research pointed out that photon-counting CT kept an accuracy rate exceeding 90 percent for these stenotic diseases. In contrast, conventional CT scans, as reported in previous studies, typically achieve around 70 percent accuracy.
Moreover, PC CTA excelled in diagnosing stenotic disease in the iliac artery segments. Here, PC CTA achieved 95 percent sensitivity, 98 percent specificity, and 98 percent accuracy, suggesting that PC CTA may be particularly advantageous for detecting stenosis in larger, proximal vessels. The pure lumen reconstructions with PC CTA also received high marks in iliac segments, showing 93 percent sensitivity, 94 percent specificity, and 93 percent accuracy.
Dr. Ghibes emphasized the reliable diagnostic image quality of PC CTA, highlighting its effectiveness in detecting high-grade stenosis even in particularly challenging calf arterial segments. Despite these promising results, the study did acknowledge certain limitations, including a possible patient selection bias as most participants had a history of PAD, possibly skewing the results due to a limited representation of those with less severe forms of the disease. Additionally, comparisons between photon-counting CTA and other technologies such as multidetector CT and dual-energy CT were not included in this study.
PC CTA appears to hold considerable promise as a non-invasive diagnostic tool for stenotic lesions in patients with peripheral artery disease, offering a potentially safer and similarly effective alternative to more invasive methods like DSA. This advancement may mark a significant shift in how medical professionals approach the diagnostic process for vascular diseases, providing clearer images and differentiated details that were once challenging to obtain.