Recent scientific research has uncovered that lesions detectable by prostate-specific membrane antigen (PSMA) can be found in over three-quarters of men experiencing an increase of less than 2 ng/ml in prostate-specific antigen (PSA) levels after undergoing radiotherapy for prostate cancer. This discovery is shedding light on how these lesions could play a crucial role in managing prostate cancer recurrences more effectively.
Published in the journal European Urology Oncology, the study pulls from a database of 568 patients who received curative radiotherapy for prostate cancer. Within this group, 346 individuals showed signs of biochemical recurrence as defined by the Phoenix criteria, indicating their PSA levels had risen above 2 ng/ml from the lowest point recorded post-treatment. Meanwhile, another 222 patients displayed PSA increases that remained below this mark.
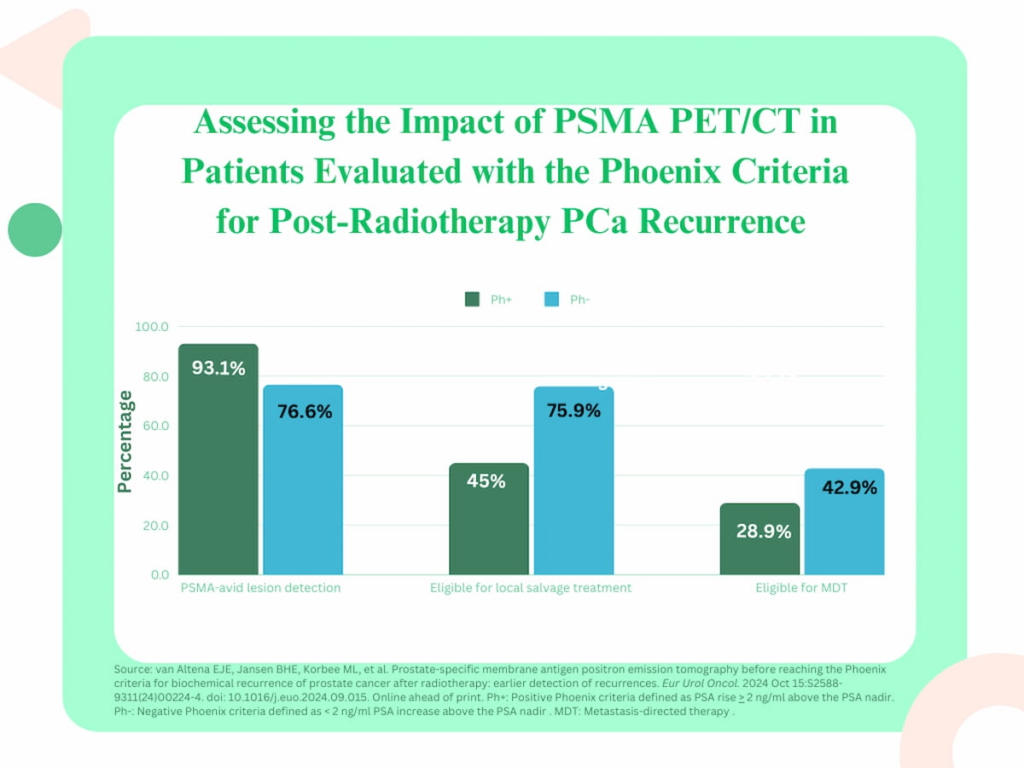
Intriguingly, the researchers identified PSMA-avid lesions in 76.6% of the group not meeting full biochemical recurrence criteria (those with a PSA rise less than 2 ng/ml), and in 93.1% of the patients who did. It was noted that among those with these lesions, a significantly larger portion of the patients who had less pronounced PSA increases were eligible for localized salvage treatments compared to their counterparts with larger PSA rises – 75.9% versus 45%, respectively. Furthermore, patients with PSMA-avid lesions who did not meet the full criteria for biochemical recurrence also showed higher eligibility for metastasis-directed therapies (MDT) compared to those who did (42.9% vs. 28.9%).
Dr. Evelien J.E. van Altena from the Department of Urology at Amsterdam University Medical Centers, along with her colleagues, pointed out that using PSMA PET/CT imaging at an early stage can detect the recurrence of prostate cancer when the disease is still relatively less advanced. This early detection allows for timely intervention through salvage treatment or MDT.
Additionally, the study’s five-year follow-up results indicated that 33% of the men in the group with less dramatic PSA increases needed to restart androgen deprivation therapy (ADT) compared to a much higher percentage (67.6%) in the full biochemical recurrence group. Furthermore, progression to castration-resistant prostate cancer was more than twice as frequent in the full recurrence group compared to the group with lesser PSA rises (27.9% vs. 13.6%).
The researchers also highlighted three key insights from their findings:
-
Higher Detection Rates: The PSMA PET/CT imaging allowed for an impressive rate of PSA-avid lesion detection even in cases of mild PSA increases, thus identifying potential recurrences earlier.
-
Increased Treatment Eligibility: Patients experiencing lesser increases in PSA levels after radiotherapy were more likely to qualify for salvage treatments, offering them better prospects for addressing their cancer reappearance locally.
- Improved Patient Outcomes: These patients with lower PSA increases benefited from delayed need for ADT, reduced likelihood of progression to more severe prostate cancer forms, and ultimately, extended overall survival times.
In conclusion, the study reported a noteworthy extension of survival time by an average of 22 months for those in the less severe PSA increase group compared to the full biochemical recurrence group. These outcomes suggest significant benefits associated with early PSMA imaging, potentially leading to more strategic and beneficial management of prostate cancer.
Still, the authors noted limitations to their study, primarily around the retrospective and non-randomized nature of the research. This brings potential concerns about bias in patient selection given the absence of standardized criteria for PSMA PET/CT utilization and ADT application across the cohort. Moreover, a lack of specific data about causes of death made it challenging to pin survival rate improvements directly to changes in disease management.
These findings pave the way for more targeted investigations that could further clarify the role of early PSMA PET/CT imaging in the proactive treatment of prostate cancer, potentially adapting clinical practices to focus resources on patients showing early-stage recurrence signs before more severe clinical symptoms appear.