Recent findings in interventional radiology underscore the significant impact genicular artery embolization (GAE) can have on alleviating symptoms and improving life quality for individuals enduring moderate to severe knee osteoarthritis (OA). This insight is based on a retrospective study shared at the Radiological Society of North America (RSNA) conference, which evaluated the effectiveness of GAE in 167 patients, predominantly around 69 years of age.
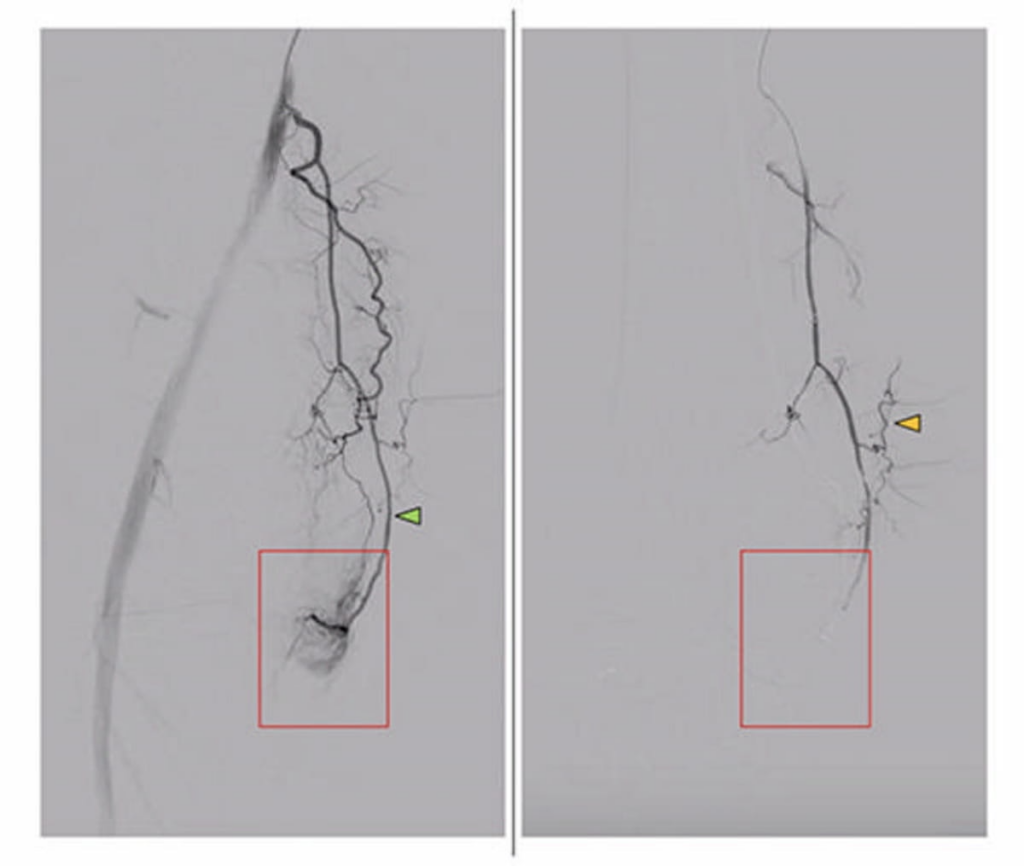
Within the studied group, almost half were diagnosed with stage 4 knee OA, while roughly 41 percent exhibited stage 3 conditions. Using digital subtraction angiography, researchers identified specific blood vessels linked to the pain reported by patients, targeting these for embolization.
Before and after images from the pre- and post-embolization processes demonstrate notable changes. For instance, in a patient with symptomatic knee OA, the genicular artery displayed a hyperemic blush indicative of increased blood flow prior to embolization—this is notably absent in post-procedure imaging, showcasing the procedure’s potential effectiveness in addressing inflammation and pain.
The study employed the Knee Injury and Osteoarthritis Outcome Score (KOOS) and found a significant 87 percent boost in patients’ quality of life after six months. Complementarily, the visual analog scale (VAS) showed a 71 percent enhancement in pain perception. Although there were instances of mild skin discoloration and knee discomfort following GAE, no severe adverse effects were reported.
Dr. Florian Nima Fleckenstein, the lead author and an interventional radiologist from Charite — University Hospital Berlin, highlighted the transformative potential of GAE. He noted that the treatment notably alleviates knee pain and significantly enhances life quality shortly after the procedure, with sustained benefits, especially for those who haven’t benefitted from other treatments like physical therapy or medication. He emphasized that GAE could offer renewed hope and improved mobility to many suffering from OA-related challenges.
While large-scale studies are still needed, the researchers advocate that GAE presents a viable, non-invasive treatment option characterized by lower complication rates and costs, simultaneously elevating the sufferers’ quality of life. Moreover, Dr. Fleckenstein posits that GAE could reduce the need for invasive surgeries and associated healthcare expenses, broadening its potential utility as a treatment for knee osteoarthritis.
The preliminary results from this study fuel optimism about incorporating GAE as a mainstream alternative in combating knee osteoarthritis, particularly for its potential to alleviate pain, enhance mobility, and streamline treatment costs.