Recent research highlights the potential of prostate-specific membrane antigen positron emission tomography (PSMA PET) in improving the detection of metastasis in patients facing recurrence of prostate cancer (PCa). This advanced imaging technique appears not only to enhance the quality of life for these patients but may also lead to lower mortality rates when compared to traditional imaging approaches.
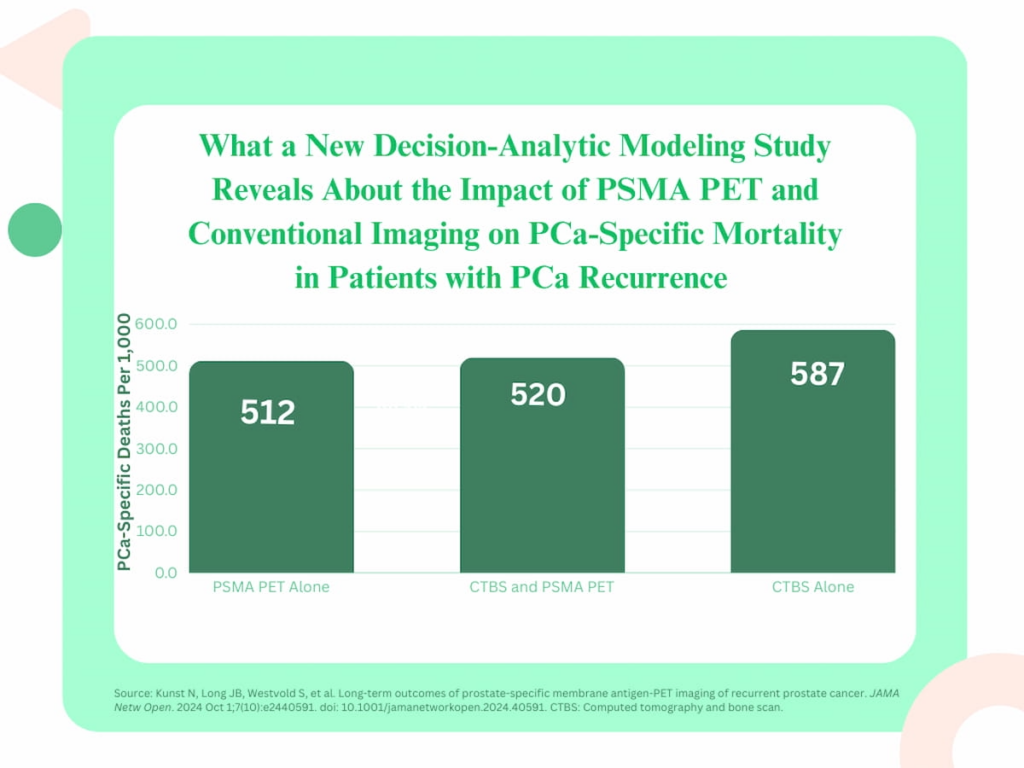
A study published in JAMA Network Open conducted a decision-analytic modeling assessment to compare long-term outcomes from three methods of imaging: immediate PSMA PET use, conventional computed tomography and bone scans (CTBS) followed by PSMA PET for inconclusive findings, and CTBS alone. The focus was on simulated patients experiencing biochemical recurrence (BCR) of prostate cancer.
The findings were significant. Among 1,000 simulated patients diagnosed with PCa BCR, the immediate application of PSMA PET revealed metastatic disease in 611 cases, which is more than double the 297 diagnoses made through CTBS alone. Interestingly, a combination of CTBS followed by PSMA PET managed to detect metastasis in 630 patients, indicating that while CTBS can be useful, PSMA PET is far more effective in identifying cancer spread.
Moreover, the study also looked at the impact of PSMA PET on mortality rates. It was estimated that using this imaging technique could prevent 75 prostate cancer-specific deaths for every 1,000 patients in comparison to CTBS, which resulted in 587 deaths. When juxtaposed with the CTBS and subsequent PSMA PET combination, PSMA PET alone still showed a reduction of eight deaths, making it a crucial diagnostic tool in patient management.
The researchers projected that the exclusive use of PSMA PET would accumulate about 8,741 quality-adjusted life years (QALYs), compared to 8,609 QALYs with the CTBS and PSMA PET combination and 7,917 QALYs resulting from CTBS alone. Such statistics underline an essential improvement in the quality of life and overall patient outcomes when utilizing PSMA PET.
Lead author Natalia Kunst, Ph.D., associated with the University of York and Yale School of Medicine, emphasized that employing PSMA PET either by itself or as a follow-up test after conventional imaging yields a significant increase in the detection of metastatic diseases, thereby facilitating the commencement of systemic therapy for over 60% of the patients assessed.
Notably, the effectiveness of PSMA PET imaging particularly stands out for patients with prostate-specific antigen (PSA) levels exceeding 5 ng/mL, where the differences in detection rates become even more pronounced.
To summarize the study’s key takeaways:
-
Enhanced Metastasis Detection: PSMA PET has proven to detect more than twice the number of prostate cancer metastases compared to CTBS, marking a considerable advancement in early detection strategies.
-
Superior Quality of Life Outcomes: The application of PSMA PET is associated with improved health outcomes, yielding 8,741 QALYs over CTBS’s lower counts.
- Reduced Mortality Rates: The use of PSMA PET is linked to fewer prostate cancer-specific deaths, showcasing a critical advantage in patient care and survival prospects.
Additionally, the study highlights that using PSMA PET results in an increase of 1,035 life-years and 856 more QALYs per 1,000 simulated patients with BCR compared to traditional methods. This increases the urgency for clinicians to adopt PSMA PET imaging, especially in patients with elevated PSA levels where traditional imaging methods fall short.
Despite these promising results, the authors acknowledged some limitations in the study. The clinical trials that informed their model did not specify metastasis definitions for PSMA PET, and mainly involved patients with lower PSA levels that could skew the results when generalizing to a broader patient population.
In conclusion, the emerging evidence firmly positions PSMA PET as a transformative tool in prostate cancer management, particularly evident in its ability to enhance detection, improve quality of life, and reduce the rate of cancer-specific deaths among patients. The findings encourage a reevaluation of current imaging practices in favor of this promising technology.