A recent study suggests that the way mammography readings are organized, particularly in relation to breast density, could lead to more efficient workflows and reduced reading times for radiologists. This research, published in the journal Radiology, examines how the order of reviewing mammogram worklists affects the reading process.
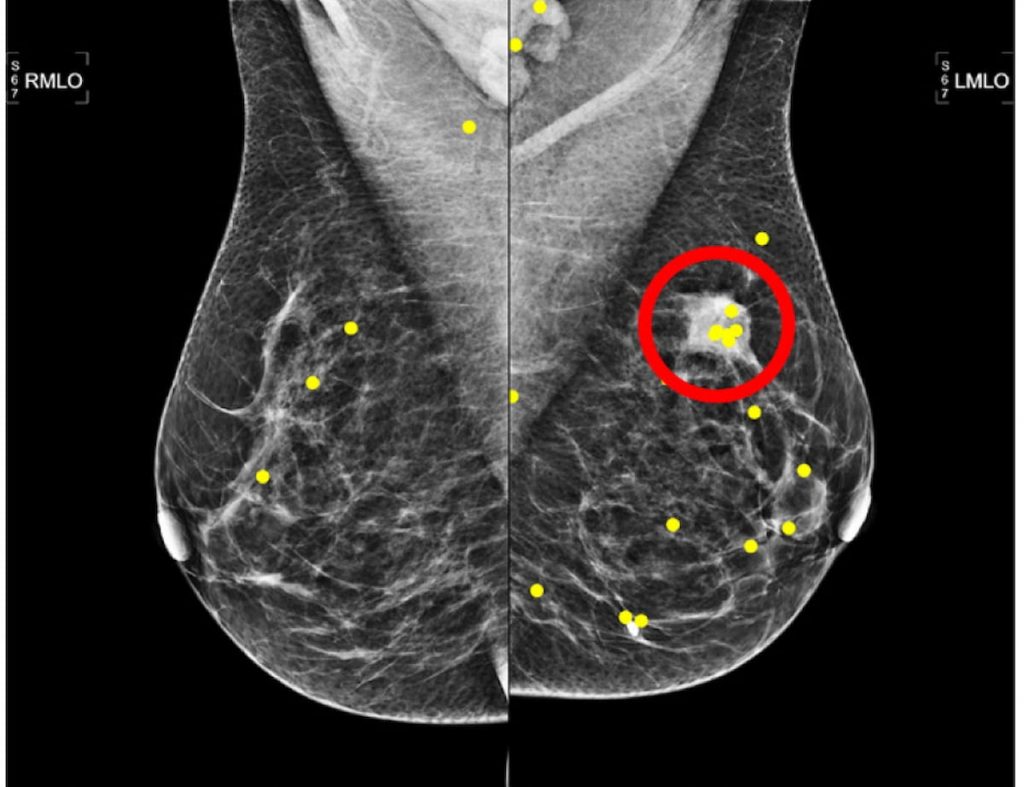
The study involved a retrospective analysis conducted by researchers at the Radboud University Medical Center in Nijmegen, the Netherlands. They compared three different methods of organizing mammography reviews: readings in order of increasing volumetric breast density (VBD), a random order, and a method using self-supervised learning (SSL), which automatically groups similar mammography images. Thirteen radiologists participated in the study, examining mammograms from a sample of 150 women, with an average age of 55, half of whom had been diagnosed with breast cancer.
The findings reveal that while organizing mammography readings by increasing VBD resulted in similar sensitivity (81% for both VBD and random orders) and specificity (86% for random vs. 89% for VBD), there were notable improvements in efficiency. Specifically, the mean reading time decreased from 27.9 seconds with random ordering to 24.3 seconds with the VBD method. Moreover, the time spent focusing on malignant regions showed a reduction from 4.6 seconds to 3.7 seconds when utilizing the VBD approach instead of random ordering.
Lead author Jessie J.J. Gommers highlighted that integrating quantitative density metrics into the mammography screening workflow could be quite beneficial. The team believes that organizing readings from low to high VBD may optimize breast cancer screening efficiency, which could be critical for improving patient outcomes.
Furthermore, the study revealed no significant variations between the SSL approach and the random order concerning sensitivity (80% vs. 81%), specificity (84% vs. 86%), or the area under the curve (AUC), which remained at 92% for both methods. Additionally, the researchers found no differences in the time to first fixation (TTFF) on lesions across the three ordering approaches.
The researchers also discussed how visual adaptation may enhance the efficiency of mammogram readings. This adaptation could help radiologists delineate between normal characteristics and unexpected anomalies in images. However, accurately identifying lesions involves more complex cognitive processes, including pattern recognition, knowledge of lesions, and clinical experience.
Key Takeaways:
-
Improved Efficiency: Using an increasing VBD order for reading mammograms could reduce average reading and fixation times, enhancing workflow efficiency without sacrificing diagnostic accuracy.
-
No Significant Diagnostic Impact: The different ordering methods, including VBD and random, demonstrated no significant differences in diagnostic performance metrics.
- Future Research Potential: While the study found no differences among reading approaches regarding TTFF or lesion detection, further research into integrating VBD into mammography workflows, particularly for techniques like digital breast tomosynthesis (DBT), could be valuable due to longer reading times associated with DBT.
In an editorial accompanying the study, Dr. Lars J. Grimm praised the researchers’ work and emphasized the potential for significant efficiency improvements with DBT, where reading times can be significantly longer than those for traditional 2D mammography. He highlighted the logistical challenges faced by high-volume breast imaging practices and the need for effective strategies to optimize interpretation times.
However, the authors acknowledged certain limitations in their study, including a focus on a cancer-enriched cohort and the lack of access to prior mammograms. They also pointed out that the emphasis on visual lesion location might have influenced results in cases where biopsy information was missing.
In summary, the study presents promising insights into how organizing mammography readings by breast density could shape future breast cancer screening practices, potentially benefitting both radiologists and patients alike.