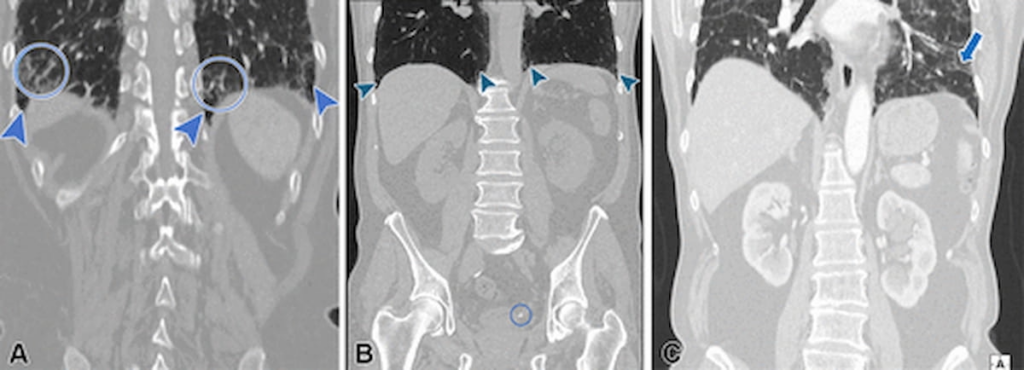
Recent findings indicate a significant oversight in the reporting of interstitial lung abnormalities (ILAs) on computed tomography (CT) scans that are initially conducted to assess abdominal or thoracoabdominal areas. In a study recently published in the journal Radiology, researchers undertook a retrospective review of 21,118 patients with an average age of 72, who had undergone these types of CT scans, to assess the prevalence and reporting accuracy of ILAs.
The study revealed that ILAs were present in 362 patients, accounting for 1.7 percent of the total sample. However, a concerning finding was that in 158 cases, ILAs were not mentioned in the original CT reports, despite being detected, resulting in an underreporting rate of 43.9 percent.
To understand this discrepancy further, the research team, led by Dr. Nicola Sverzellati from the University of Parma, explored several possible reasons why ILAs could be overlooked during radiological evaluations. They suggested that the purpose for which the CT scan was requested—often to investigate abdominal issues in clinical settings like emergency departments—might draw attention away from potential lung abnormalities. Furthermore, the absence of parenchymal window reconstruction in abdominal CTs and the subtle nature of these pulmonary changes, particularly in an older demographic, could lead to such oversights.
This issue of underreporting was notably more pronounced in abdominal CT scans, which had a 72.7 percent omission rate, compared to thoracoabdominal CTs, where the rate was significantly lower at 29.3 percent. Within these missed reports, the study identified instances where various types of ILAs went unreported: 41 percent of non-subpleural ILAs, 55 percent of subpleural non-fibrotic ILAs, and 39.3 percent of subpleural fibrotic ILAs were not documented.
Additionally, the existence of fibrotic features in over half (61.3 percent) of the patients with ILAs heightened the clinical relevance of these findings. These features were linked to a quadrupled risk of mortality attributable to respiratory causes, excluding lung cancer, marking an important clinical consequence of the lack of reporting.
Sverzellati and his team emphasized that fibrotic characteristics on CT scans, such as traction bronchiectasis, were strongly associated with the progression of ILAs and an elevated risk of respiratory-related deaths. This aligns with prior research, underscoring the necessity for precise detection and timely reporting of these fibrotic features to better manage patient outcomes.
The authors candidly recognized certain limitations inherent to their study, including the retrospective design centered on a single location and a patient group predominantly composed of White individuals. They also noted that evaluations based at baseline using either abdominal or thoracoabdominal CTs, versus the high spatial resolution CT commonly employed in follow-up scenarios, could influence assessments of the progression or improvement of ILAs.
To conclude, this study illustrates a significant gap in the standard reporting practices of ILAs in abdominal and thoracoabdominal CT exams, a gap that warrants attention in order to enhance clinical outcomes and guide appropriate management strategies for affected patients.