For patients grappling with metastatic castration-resistant prostate cancer (mCRPC), new insights from imaging technology may hold the key to better evaluating how individuals respond to treatment. A recent study, published in the Journal of Nuclear Medicine, delved into how findings from single-photon emission computed tomography/computed tomography (SPECT/CT) could offer prognostic details crucial for measuring patient outcomes when treated with ^177Lu-PSMA-617, a therapy developed by Novartis.
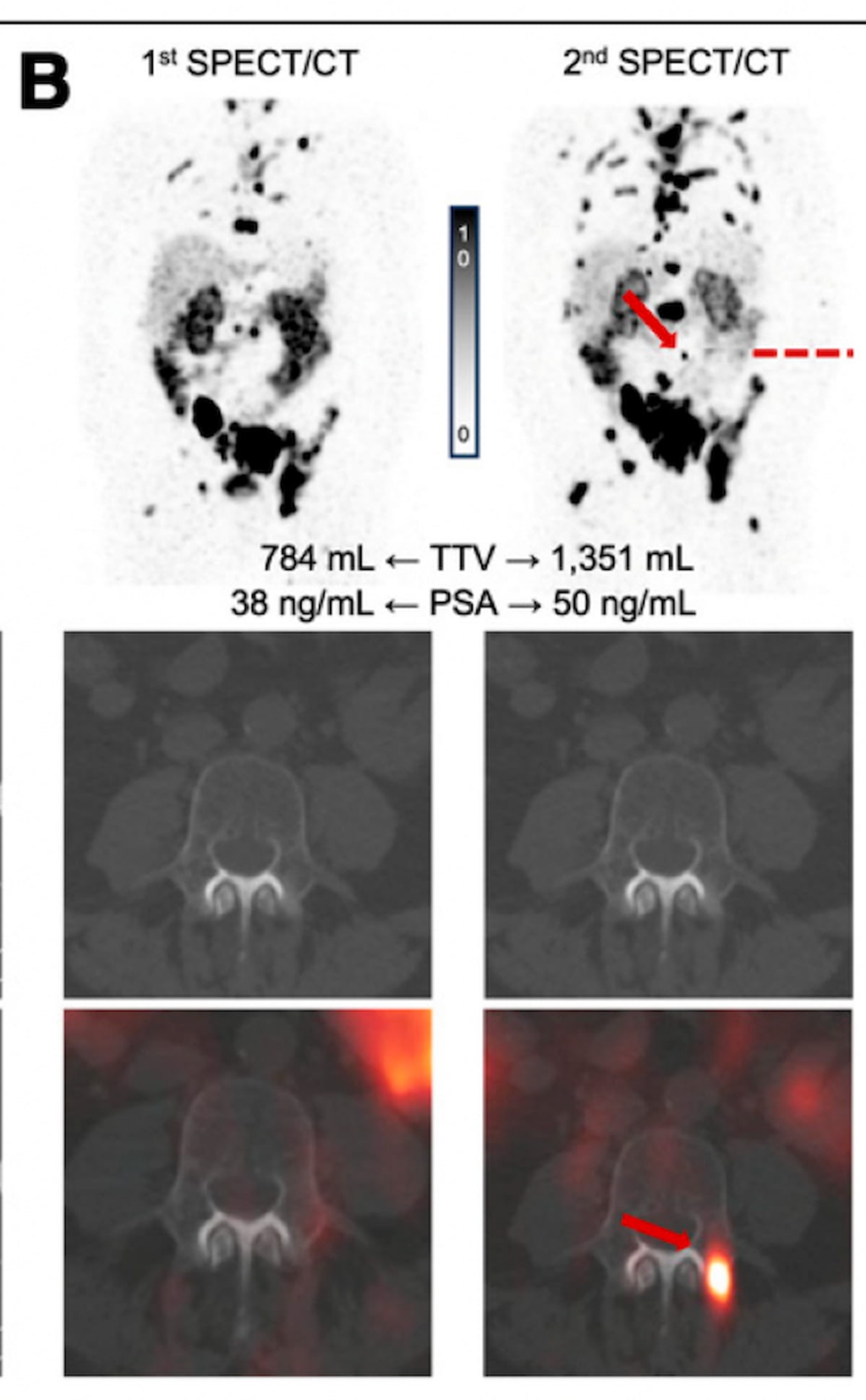
This study examined how changes in total tumor volume (TTV) and the emergence of new lesions observed on SPECT/CT scans before the second and third rounds of treatment could signal patient survival outcomes. The researchers conducted a retrospective assessment involving 66 patients, with a median age of 74, all contending with mCRPC. The patients also had a median prostate-specific antigen (PSA) level of 109 ng/mL. Tragically, 24 patients, representing 36% of the cohort, passed away before the study’s results were ready for analysis.
Delving deeper, the study noted that before commencing the second treatment cycle, 13 patients—or 20% of the group—exhibited new lesions. Additionally, 10 of these individuals saw an uptick in TTV, with seven experiencing increases exceeding 20%. Moving to the third treatment cycle, 22% of the remaining patients showed new lesions, while seven reported heightened TTV.
One intriguing aspect highlighted by the research is how higher TTV and the formation of new lesions at the start of subsequent treatment cycles correlated with increased mortality risks. Images from the study showcased cases where patients had several new PSMA-avid bone lesions by the time they began the second treatment cycle, along with a rise in TTV.
The multivariable analysis reflected that new lesions seen on SPECT/CT prior to the second and third treatment cycles were associated with elevated hazard ratios for overall survival—7.67 and 5.50, respectively. Furthermore, TTV increases before both treatment cycles correlated with hazard ratios of 2.37 and 2.19, respectively, for overall survival.
The study’s lead author, Dr. Ridvan Arda Demirci from the University of Washington’s Department of Radiology, emphasized the need for early predictors of treatment response and disease progression, given the relatively brief survival span typical for these patients. The study identified that both higher TTV and the appearance of new lesions at the initiation of treatment cycles two and three independently related to reduced overall survival, even when considering PSA changes relative to baseline.
Notably, before the second treatment cycle, 46% of new lesions involved bones, with 23% found in the liver and a mix of liver and bone lesions accounting for 31%. As patients moved to the third cycle, the figures adjusted slightly, with 55% of new lesions in bones and 36% in the liver.
The findings underline the potential of SPECT/CT imaging as a tool for crafting personalized treatment plans for advanced prostate cancer, though additional research is necessary to verify these associations and improve therapeutic strategies. Patients with substantial disease volume at the start of subsequent cycles might require more vigorous treatment approaches, such as heightened administered activity or more frequent dosing. Conversely, those with new yet low PSMA expression lesions might benefit more from combined systemic treatments or interventions targeting specific disease areas.
While emphasizing the significance of their findings, the authors also recognized the study’s limitations, including the retrospective nature and challenges related to treatment toxicity and access to radiopharmaceuticals. Additionally, the research did not incorporate pre-treatment imaging data or clinical factors within its multivariable analysis.
Overall, the study highlights the crucial role of SPECT/CT in influencing how healthcare providers might approach the management of prostate cancer, stressing the need for careful consideration of individual patient needs and potential adaptations in treatment plans based on imaging findings.