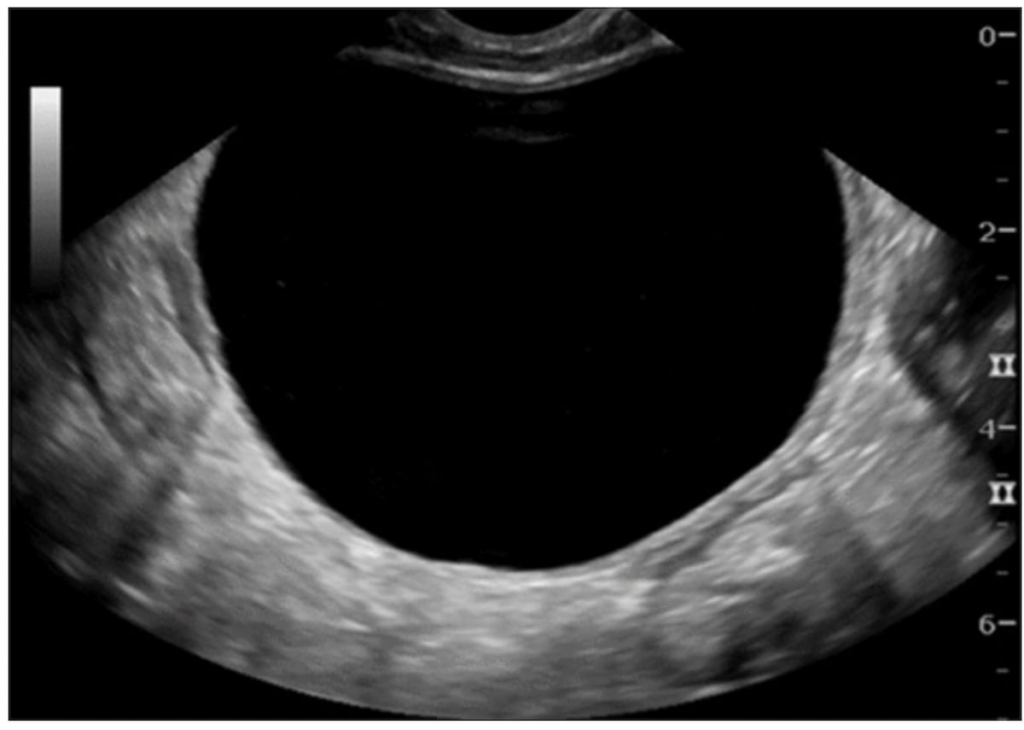
The recent findings from a multicenter retrospective study present promising insights into the use of the Ovarian-Adnexal Imaging Reporting and Data System (O-RADS) ultrasound (US) risk scoring system. This research suggests that employing O-RADS risk ratings could significantly decrease the number of unnecessary surgeries performed on women with ovarian cystic lesions who do not exhibit acute symptoms.
Published in the journal Radiology, the study examined preoperative ultrasound images from 377 patients, predominantly females around the age of 45, who had been diagnosed with ovarian cystic lesions and had undergone surgical intervention between January 2011 and December 2014. The intention was to explore how the O-RADS risk scoring system could be applied to this demographic to better inform treatment decisions.
The investigation revealed that 157 of the recorded lesions, approximately 42 percent, would have been categorized as having an O-RADS US 2022 risk score of 2. Notably, 54 percent of these lesions were identified as non-neoplastic, while 45 percent comprised benign tumors, including dermoids. Dr. Luyao Shen, the study’s lead author from Stanford University School of Medicine, noted that had the O-RADS system been utilized for these patients, almost half could have been offered conservative treatment options or follow-up imaging instead of proceeding directly to surgery.
The study highlighted the effectiveness of using an O-RADS US 4 score as a threshold for detecting malignant lesions, achieving a 94 percent sensitivity rate and a 98 percent negative predictive value (NPV). This indicates that the O-RADS system is robust in ruling out malignant diagnoses. However, researchers also caution that the system has inherent limitations, particularly regarding specificity and positive predictive value (PPV). Specifically, the O-RADS US system exhibited a specificity of 64 percent and a PPV of only 38 percent, complicating its utility in predicting malignancy accurately within this patient group.
The findings of the research underscore three core takeaways:
-
Reduction of Unnecessary Surgeries: Implementing the O-RADS US 2022 risk stratification could potentially spare nearly half of the patients from undergoing surgery, as alternative management options could be explored.
-
High Sensitivity and Negative Predictive Value: The O-RADS US 4 classification demonstrated its reliability in ruling out malignancy with impressive sensitivity and NPV rates.
- Limitations in Specificity: Despite its effectiveness in excluding malignancy, the O-RADS system’s lower specificity and PPV suggest that additional imaging modalities, such as MRI, may offer better characterization of cystic lesions.
An editorial accompanying the study by Dr. Laure S. Fournier praised the research for its originality in examining the O-RADS system’s practical application in managing ovarian lesions. She noted that while O-RADS US has its limitations, MRI could enhance the assessment of lesions classified as O-RADS US 2 and those with higher risk ratings, allowing for a more accurate diagnosis. Dr. Fournier emphasized the importance of MRI in identifying specific histologic types, which helps prepare surgeons and appropriately inform patients about potential findings before surgery.
It is important to note some limitations of the study itself. The excluded participants with acute symptoms might have skewed the results, leading to an overestimation of the PPV in the surgical cohort. Furthermore, it was indicated that the ultrasound scans were performed by technologists without specialized training in gynecologic imaging, which could impact the overall accuracy of the findings when contrasted with practices where trained gynecologic specialists are involved.
In conclusion, the study offers valuable insights into how the O-RADS ultrasound risk score can aid in clinical decision-making and effectively reduce unnecessary surgical interventions in women with ovarian cystic lesions. Future studies may further refine these findings, improving the management strategies for patients presenting with such conditions.